- Monday to Sunday 08:00 - 20:00
- +353 (0)1 267 8011
- info@healthcareabroad.ie
Bariatric Surgery
At Healthcare Abroad, we offer bariatric surgery using a structured approach that prioritizes patient care before, during, and after surgery. This method ensures safe, effective weight-loss procedures and puts you on the right path for long-term success.

Preparing for Your Bariatric Journey
Embarking on a journey towards improved health through bariatric surgery requires a seamless process to ensure your comfort and well-being. Here’s a step-by-step guide to help you navigate the stages before your travel:
- Identification of Treatment Need-Your first step is to consult with your GeneralPractitioner (GP) or consultant who will assess and identify the necessity for bariatric surgery.
- Initiate Contact with Healthcare Abroad– Once the need for treatment is established, either you or your GP can initiate contact with Healthcare Abroad. Our dedicated team is ready to guide you through the process of receiving surgery in an EU country under the cross border directive.
- Referral and Diagnostic Coordination-The Healthcare Abroad team will collaborate with your GP to arrange a referral letter from your GP. We streamline this process by providing the results directly to the chosen hospital.
- Hospital and Surgeon Matching– Our team, with a vast network of hospitals and skilled surgeons, will carefully match your requirements to ensure you receive personalised care.
- Financial Assistance– If needed, we can assist you in organising your finances through Irish credit unions, making the financial aspect of your healthcare journey hassle-free.
- Surgery Planning and Documentation– Coordinating with the selected hospital, we facilitate the arrangement of surgery dates and ensure all necessary files are sent for review.
- Confirmation of Travel Dates– Once your healthcare plan is confirmed, we liaise with the hospital team to finalise your travel dates and healthcare schedule.
- Scheduling a meeting with our dietitian: Who will help you with pre-travel nutrition care pathway please see section below for more details.
- Meeting with our psychologist for an evaluation – more info below.
- Arrival and Out-Patient Appointment– Upon arrival at the hospital, you’ll have an out-patient appointment with your consultant the day before the scheduled treatment, ensuring all pre-operative concerns are addressed.
- Post-Surgery Paperwork– After your surgery, we take care of finalising all paperwork, submitting it to the Health Service Executive (HSE) on your behalf, and ensuring a prompt refund process.
- Report to Local GP– To maintain continuity of care, your GP will receive a comprehensive report from the hospital regarding the treatment received, updating your local medical records accordingly.

Why Choose Healthcare Abroad for Bariatric Surgery?
1. Skip the Long Waiting Lists
In Ireland, patients often wait years for bariatric surgery. With Healthcare Abroad, you can have your procedure in just a few weeks, giving you a head start on your health journey.
2. Expert Surgeons and Hospitals
We work with 86 internationally accredited private hospitals across Europe, giving you access to top bariatric surgeons and world-class care.
3. Comprehensive Care Made Easy
We take care of everything:
- GP referral letters
- Hospital appointments
- Free transfers between your accommodation and the hospital
4. Fully Reimbursed Treatment
Under the EU Cross Border Directive, the HSE fully reimburses the cost of your surgery. We handle all the paperwork to make the process hassle-free.
Obesity and Chronic Diseases
Overweight and obesity is defined as ”abnormal or excessive fat accumulation that presents a risk to health” (World Health Organisation, 2017). It is a progressive, chronic and complex disease affecting all ages and genders.
Measuring Obesity
Body mass index (BMI) is the most widely used measure of obesity in clinical practice as direct assessment of body fat is not readily available. BMI defined as weight in kilograms divided by the square of height in meters (kg/m2), is considered to be the best available population marker for monitoring trends in overweight and obesity in adults, children and young people over time.
Ireland has one of the highest levels of obesity in Europe, with 60% of adults and over one in five children and young people living with overweight and obesity. There are multiple drivers that influence obesity including genetics, environmental and socioeconomic factors.
Obesity is associated with other chronic diseases such as type 2 diabetes, cardiovascular disease, respiratory disease, several types of cancer, pain and musculoskeletal disorders. Certain groups in the population have a high risk of excess weight gain leading to obesity, these include older people, women in pregnancy and post-natal, individuals with eating disorders, mental illness, intellectual and physical disabilities as well as socially excluded and disadvantaged groups.
Mental Impact
Overweight and obesity is a highly stigmatized condition. Many people, including healthcare practitioners, have negative attitudes and beliefs about people with overweight and obesity. Weight stigma in healthcare can prevent healthcare professionals from having supportive and non-judgemental consultations with patients, which can result in a lack of diagnosis and low efficacy of interventions for weight management.
Experiences of judgement and shame in the healthcare setting prevents people with obesity from seeking help. Weight stigma can also lead to the under-recognition and undermanagement of symptoms of eating disorders. Stigmatisation is associated with greater psychological distress and can cause people to engage in behaviours that make obesity worse.
The complex nature of obesity requires that the health services take a holistic, integrated approach to identification, early intervention and treatment. Actively managing overweight and obesity will improve health, quality of life and overall mortality while reducing healthcare costs.
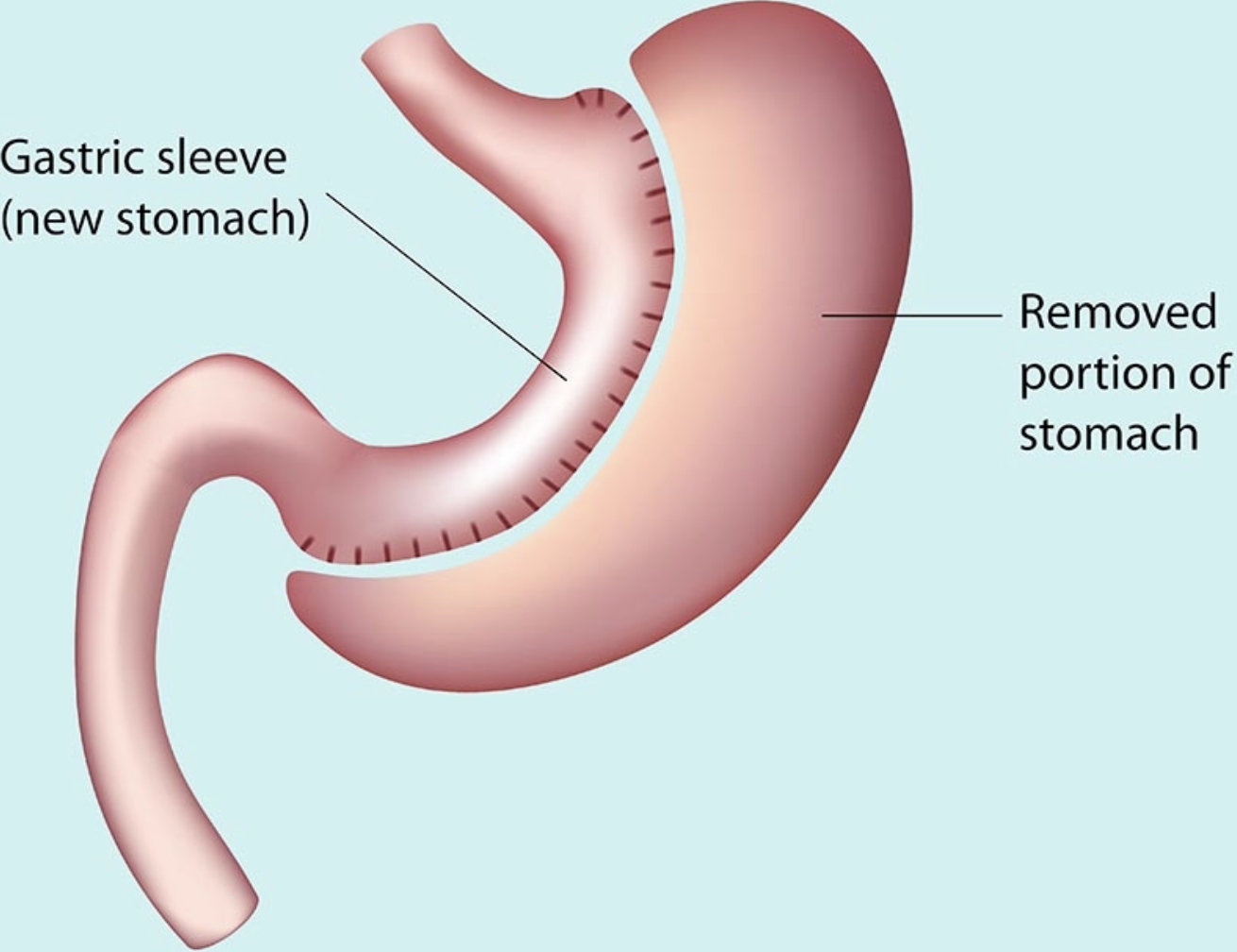
Gastric Sleeve
What is a Gastric Sleeve?
As can be seen from the image opposite, the operation requires complete removal of around 80% of the body of the stomach. This is done using a special instrument which cuts and staples at the same time. What remains of the stomach has the appearance of a sleeve – or perhaps more accurately a banana.
This is done under a general anaesthetic using keyhole surgery and takes around 1-1.5 hours to complete. A key advantage is that, unlike gastric bypass, with a sleeve gastrectomy the food you eat enters and leaves the stomach in the same way it did before surgery.
Possible Health Benefits of Gastric Sleeve Surgery
- Reduced risk of heart attack and stroke (due to lower blood pressure and cholesterol levels)
- Type 2 diabetes – Possible improvement in blood glucose management, and even remission, for people with type 2 diabetes.
- Sleep apnoea – resolution or marked improvement in snoring, daytime sleepiness and fatigue
- Back and joint pain – most people who have had bariatric surgery experience reductions in back and joint pain and markedly improved mobility.
- Stress incontinence – is common in women, and they may experience significant improvement or complete resolution of symptoms.
- Infertility and PCOS – people with polycystic ovarian syndrome (PCOS) may experience correction of underlying hormonal problems and improved fertility
- Non-alcoholic Fatty liver disease – 80% of patients will have complete resolution of obesity-associated fatty liver disease
- Psychological wellbeing – reduced depressive symptoms and anxiety, improved social interaction and overall quality of life.
How much weight will I lose?
Short term
Initial weight loss with a sleeve is high – in some studies as high as 75% of excess weight. This is one of the reasons why the gastric sleeve has become so popular; it appears to offer dramatic weight loss relatively easily and, unlike the gastric band, it seems to require minimal follow-up. However, the longer-term results are not quite so optimistic.
Longer term
Despite the dramatic early weight loss, longer-term results with the sleeve show a pattern of weight regain over time.
For example, in one study, excess weight loss at 1-year was 71% but fell to 53% at 10-years. In another published trial, excess weight loss at 1, 3,5 and 8-years, was 72, 86, 63 and 52%.
Why does this weight regain occur?
It’s probably a combination of stretching of the gastric remnant (the 20% of stomach that remains after surgery), poor dietary habits and a return of the appetite due to increasing ghrelin levels.
Risks of Gastric Sleeve Surgery
The sleeve gastrectomy is the riskiest of the available surgical weight loss procedures. The three main risks (two post-surgical and the third a later complication) are as follows:
- Bleeding – is the most common complication and occurs in roughly 1 in 200 (0.5%) sleeve patients. It may require blood transfusion and a re-operation, but it can often be managed without further surgery.
- Leakage – is the most feared complication following a sleeve operation and is due to stomach contents leaking through the long staple line. It usually occurs within the first few days following surgery, in roughly 1 in a 100 (1%) of patients. It can be difficult to manage and may require an extended stay in hospital
- Reflux – if you have a history of reflux (heartburn), then you will not be offered a sleeve gastrectomy. This is because your reflux will inevitably become much worse and you are less likely to be successful with your weight lossMoreover, a significant proportion of patients (around 9%) who did not have reflux prior to the procedure, will develop this as a direct result of the surgery. This is not a trivial issue, because chronic reflux can cause potentially serious problems in the lower gullet (oesophagus).
Am I eligible for the Gastric sleeve?
-
- Age > 20 but under 65 years
- BMI of 40kg/m² or greater (check your BMI here).
- No history of reflux (heartburn)
- No previous surgical weight loss procedures
- A full understanding of the risks and benefits of the sleeve
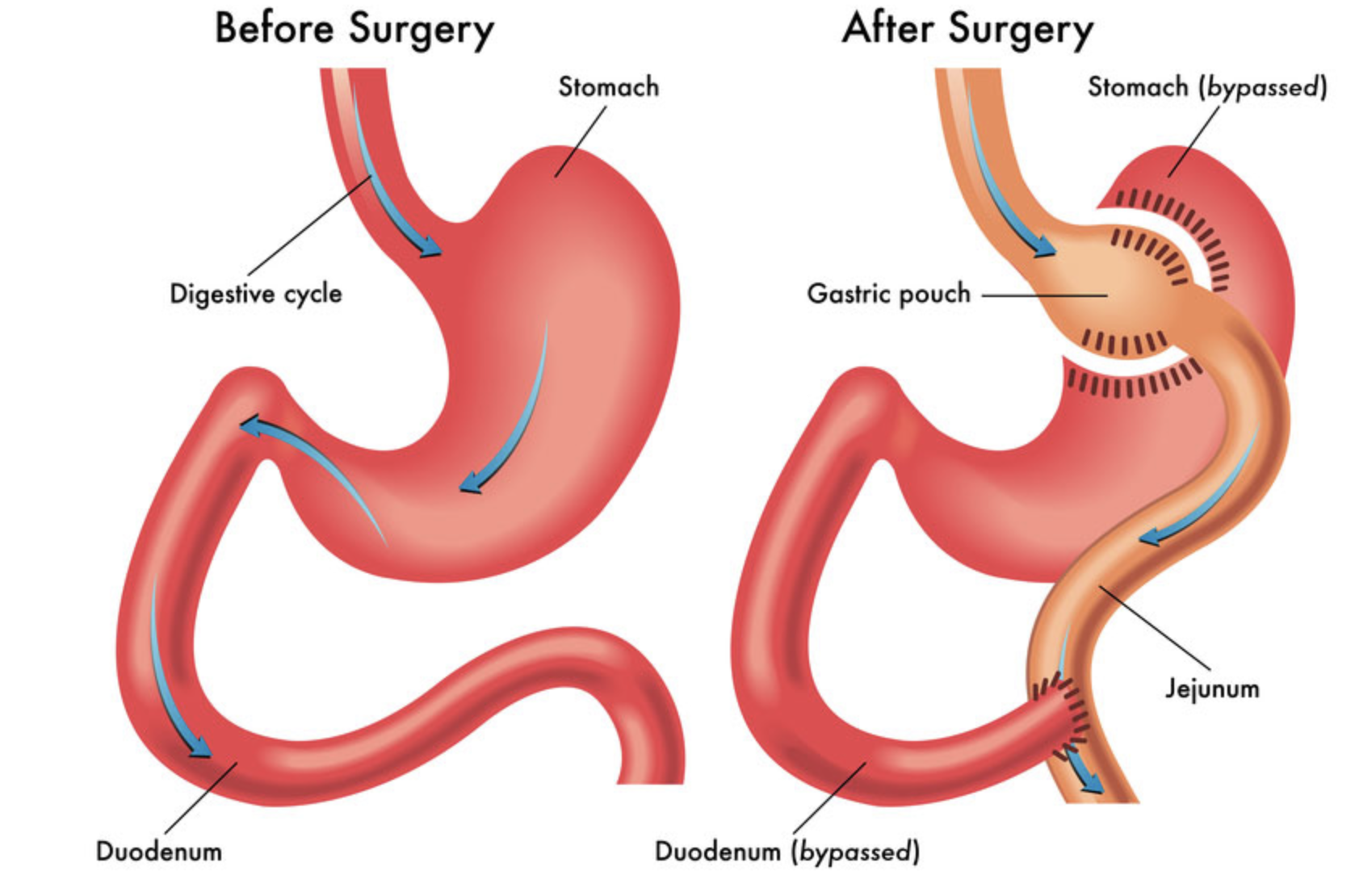
Gastric Bypass Surgery
The gastric bypass method involves connecting the uppermost part of the stomach (forming a small pouch) directly to the small intestine. After the gastric bypass, the ingested food will enter this small pouch in the stomach and then directly into the small intestine, bypassing most of the stomach and the first section of the small intestine.
Why it’s done
Gastric bypass surgery is undertaken to facilitate weight loss and diminish the likelihood of encountering severe weight-related health complications, which may include:
- Gastroesophageal reflux disease
- Heart disease
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Type 2 diabetes
- Stroke
- Cancer
- Infertility
Generally, gastric bypass surgery is pursued only after attempts to shed excess weight through dietary enhancements and exercise regimens have been made.
Who Should Consider Gastric Bypass Surgery?
Gastric bypass and similar weight-loss procedures may be suitable for individuals who meet the following criteria:
- Those with a body mass index (BMI) of 40 or higher, indicating extreme obesity.
- Individuals with a BMI ranging from 35 to 39.9 (obesity), coupled with significant weight-related health issues like type 2 diabetes, high blood pressure, or severe sleep apnea. In some instances, individuals with a BMI of 30 to 34 and serious weight-related health conditions may also qualify for specific types of weight-loss surgery.
However, gastric bypass surgery isn’t appropriate for every severely overweight person. Meeting specific medical prerequisites is necessary to qualify for weight-loss surgery. Undergoing psychological evaluation and regular consultations with a dietitian are typically part of the process.
Moreover, candidates must be prepared to commit to permanent lifestyle changes to adopt a healthier way of living. Long-term follow-up plans, encompassing nutritional monitoring, lifestyle and behavioral adjustments, as well as management of medical conditions, may also be required.
Risks
As with all major surgeries, gastric bypass and other weight-loss surgeries pose potential health risks, both in the short and long term.
Risks that are associated with the procedure are similar to any other abdominal surgery and can include:
- Excessive bleeding
- Infection
- Adverse reactions to anesthesia
- Blood clots
- Lung or breathing problems
- Leaks in your gastrointestinal system
Longer term risks and complications of gastric bypass surgery can include:
- Bowel obstruction
- Dumping syndrome, causing diarrhea, nausea or vomiting
- Gallstones
- Hernias
- Low blood sugar (hypoglycaemia)
- Malnutrition
- Stomach perforation
- Ulcers
- Vomiting
Rarely, complications of gastric bypass can be fatal.
Preparation Process
As your surgery approaches, you might need to initiate a physical activity regimen and cease tobacco and alcohol consumption. In the immediate period before your procedure, dietary restrictions and medication guidelines will be in place. It’s advisable to strategise for your post-surgery recovery now. Consider organizing assistance at home if you anticipate requiring it.
What you can expect
Gastric bypass surgery is done in the hospital. Depending on your recovery, your hospital stay is typically one to two days but may last longer.
During the Procedure
Before the commencement of your surgery, you will receive general anesthesia to ensure you remain asleep and comfortable throughout the procedure.
The specifics of your gastric bypass surgery will be tailored to your individual circumstances and the practices of your physician. While some surgeries utilize traditional large (open) incisions in the abdomen, the majority are conducted laparoscopically, involving the insertion of instruments through several small incisions in the abdomen.
Following the incisions made either through the open or laparoscopic method, the surgeon cuts across the top of your stomach, isolating it from the rest of the stomach. The resulting pouch is approximately the size of a walnut and has a capacity of holding only about an ounce of food, a significant reduction compared to the typical capacity of the stomach, which is about 3 pints of food.
Subsequently, the surgeon severs the small intestine and attaches a portion of it directly to the pouch. Food then travels into this small pouch of the stomach and proceeds directly into the section of the small intestine that has been sewn to it, bypassing most of the stomach and the initial part of the small intestine.
The surgery typically lasts for several hours. Following the procedure, you will awaken in a recovery room, where medical staff will monitor you for any potential complications.
After the Procedure
Immediately post-surgery, you will be restricted to liquids only, as your stomach and intestines begin the healing process. This will progress gradually to a special diet plan transitioning from liquids to pureed foods, followed by soft foods, and eventually firmer foods as your body adjusts.
There will likely be numerous restrictions or limitations on your diet and fluid intake post-surgery. Your doctor will advise you to take vitamin and mineral supplements, including a multivitamin with iron, calcium, and vitamin B-12.
Regular medical checkups will be necessary in the initial months after weight-loss surgery to monitor your health, possibly including laboratory tests, blood work, and various examinations.
In the first three to six months following gastric bypass surgery, you may experience changes as your body reacts to rapid weight loss, such as body aches, fatigue, feeling cold, dry skin, hair thinning or loss, and mood changes.
Results
Gastric bypass surgery can yield significant long-term weight loss, with the extent depending on the type of surgery and changes in lifestyle habits. It’s possible to lose approximately 70% or more of excess weight within two years.
In addition to weight loss, gastric bypass surgery may lead to improvements or resolution of conditions commonly associated with obesity, including gastroesophageal reflux disease, heart disease, high blood pressure, high cholesterol, obstructive sleep apnea, type 2 diabetes, stroke, and infertility. Furthermore, it can enhance your ability to perform daily activities, potentially improving your overall quality of life.
When Weight-Loss Surgery Doesn’t Work
Failure to achieve sufficient weight loss or weight regain after weight-loss surgery is possible if recommended lifestyle changes are not adhered to. Consistently indulging in high-calorie snacks, for example, may impede weight loss progress. To prevent weight regain, it’s essential to adopt permanent healthy changes in diet and maintain regular physical activity and exercise.
Adhering to all scheduled follow-up appointments post-surgery is crucial so that your doctor can monitor your progress. If you notice inadequate weight loss or develop complications following surgery, it’s important to seek medical attention promptly.

Nutritional Support
Didi de Zwarte is a registered dietitian. She has over 8 years’ experience working in various hospitals and healthcare settings in Ireland.
She has a Bsc. (first class hons) in Human Nutrition and Dietetics from Trinity College Dublin and the Technical University of Dublin. She has experience working in chronic disease, diabetes and obesity care across Ireland.
She currently works as a senior clinical dietitian in Ireland. She also works for the HSE communications division, where she researches digital tools to support those living with obesity and type 2 diabetes.
She also runs her own private practice, called Didititian. She started her practice in 2019 and she has guided numerous clients through their own weight management journeys.
She joined our team in Healthcare Abroad in early 2023, and has worked with our consultant to develop our bariatric nutritional care pathway.
Didi is passionate about fighting stigma associated with obesity. She works at national level to support appropriate communication about obesity as a chronic disease.
She makes sure her clinic is a safe and supportive space for our clients to explore their relationship with food. She provides detailed advice and support as her clients progress through the various stages of the pre and post bariatric surgery diets.
Our bariatric nutrition care pathway
Our dietitian Didi has worked with our consultant to develop a 5 Step Bariatric Nutrition Care Pathway. Didi runs a virtual clinic, and all her sessions will be over a GDPR-approved video calling platform.
Step 1: Didi will meet you around 3 weeks before surgery for a detailed initial consultation. In this session, she will learn more about your unique journey to this point. She will assess the various physical and mental aspects of your experience of living with obesity. She will then prepare a personalised pre-operation nutrition plan, which may include a diet to support “liver reduction” for some time. Each client’s journey is individual and Didi will make sure to explain each step of the journey.
Step 2: Didi will meet you around 1 week before you fly out to Spain. During this session, she will check in on your mental and physical health ahead of surgery, and offer further advice to support your health at this time. Our hospital staff will support your nutritional care while you are in the hospital in Denia.
Step 3: Didi will check in with you for a call around 6 days after your surgery to assess how you are progressing. She may offer advice to support your recovery and make any potential changes to your eating plan based on your symptoms.
Step 4: Didi will then meet you when you are back home to discuss the next steps in your eating plan, and work with you to troubleshoot any concerns or symptoms you experience.
Step 5: Didi will have one final session with you around 2-3 months after surgery. In this session, she will work with you to manage any remaining symptoms. She will support you to find a balanced and enjoyable diet that works for you. She will also offer further guidance on your longer-term follow-up.
It is recommended that you continue to work with a dietitian in the long-term, to support you with your ongoing weight management journey, and ensure your diet remains balanced and nutritious. Didi will offer guidance on this longer-term planning also.
It is important to be aware that everyone who has had bariatric surgery will need to take a range of vitamin and mineral supplements for life. This is because your body can not absorb these nutrients fully from food anymore after surgery. Didi will discuss this with you and can work with your GP to prepare prescriptions for these.

Psychotherapy & Counselling
Dónal Donnelly
Dónal is a fully accredited member of the Irish Association for Counselling and Psychotherapy (IACP). In addition to his psychological qualifications, he holds an Honours Degree and Professional Qualification in Law and a Masters in Education and Counselling from Trinity University Dublin. He has worked extensively in employment law, recruitment, career coaching and psychotherapy.
He has always been fascinated with helping others live their optimal lives. He is a firm believer in the resilience of the human spirit and the importance of providing people with crucial skills to awaken their sense of autonomy and self-determination during difficult times in their lives.
He specialise in a variety of issues including anxiety, depression, relationship issues, self-esteem issues, obsessive thinking patterns, intrusive thoughts, grief, trauma, couples issues, separation processes, workplace stress, work-life balance, workplace assertiveness, and workplace bullying.
He brings an optimistic, non-judgmental approach to therapy and use a variety of modalities including humanistic, person-centred, psychodynamic, existential and CBT. In addition, he is highly experienced in the solution-focused model, which is best suited for the EAP referral system.
His unique, diverse background, experience and qualifications equip him with a range of specialist skills that can help his clients bring balance to their lives and overcome the hurdles that prevent them from reaching their true potential.
Certifications
- IICP (Institute of Integrative Counselling and Psychotherapy). Professional Counselling and Psychotherapy qualification.
- Trinity College Dublin. (Masters in Education, Guidance and Counselling).
- Trinity College Dublin. (Psychology and French. Bachelor of Laws; LL.B.).
After returning home
Following bariatric surgery, it’s crucial for patients to adhere to a comprehensive aftercare plan to ensure successful weight loss and long-term health. Here are some follow-up aftercare tips for patients:
- Dietary Guidelines: Stick to the prescribed diet plan provided by your healthcare team. Initially, this may involve consuming liquids and gradually transitioning to soft foods and then solid foods. Pay attention to portion sizes and avoid high-calorie, high-fat, and sugary foods.
- Hydration: Drink plenty of water throughout the day to stay hydrated. Aim for at least 8 cups of water per day, but your specific needs may vary depending on factors such as activity level and climate.
- Vitamin and Mineral Supplementation: Bariatric surgery can impact the body’s ability to absorb certain vitamins and minerals. Take prescribed supplements, including multivitamins, calcium, vitamin D, vitamin B12, and iron, as recommended by your healthcare provider.
- Physical Activity: Gradually incorporate physical activity into your daily routine as advised by your healthcare team. Start with low-impact exercises such as walking and gradually increase intensity and duration over time. Regular exercise not only aids in weight loss but also promotes overall health and well-being.
- Regular Follow-up Appointments: Attend all scheduled follow-up appointments with your healthcare provider. These appointments are essential for monitoring your progress, addressing any concerns or complications, and making necessary adjustments to your treatment plan.
- Behavioral Support: Seek support from a therapist, counselor, or support group specializing in bariatric surgery. Behavioral counseling can help you navigate emotional challenges, develop healthy coping mechanisms, and maintain long-term lifestyle changes.
- Monitor for Complications: Be vigilant for signs of complications such as nausea, vomiting, abdominal pain, or difficulty swallowing. Contact your healthcare provider immediately if you experience any concerning symptoms.
- Lifestyle Changes: Embrace lifestyle changes that promote overall health and well-being, including adequate sleep, stress management techniques, and avoiding unhealthy habits such as smoking or excessive alcohol consumption.
- Mindful Eating: Practice mindful eating techniques such as chewing slowly, savoring each bite, and listening to your body’s hunger and fullness cues. Avoid distractions such as television or electronic devices while eating.
- Patience and Persistence: Understand that weight loss following bariatric surgery takes time and requires patience and persistence. Celebrate your progress, no matter how small, and stay committed to your long-term health goals.
By following these aftercare tips and maintaining open communication with your healthcare team, you can maximize the benefits of bariatric surgery and achieve long-term success in managing your weight and improving your overall health.
